Abstract
Introduction
Since the advent of chemo-immunotherapy, diffuse large B-cell lymphoma (DLBCL) is one of the few haematological malignancies that is considered potentially curable, with the life-expectancy of patients who respond to therapy returning to background general population levels. Few studies have, however, examined the veracity of this assumption. With centralised diagnostics and a unified clinical network covering a catchment population of 4 million people, the UK's Haematological Malignancy Research Network (HMRN) was specifically established to provide timely real-world data to answer such questions; and findings from this unique population-based cohort are reported here.
Methods
Demographic, prognostic, treatment and outcome data were examined for all patients (18+ years) newly diagnosed 2004-15 with de novo DLBCL (n= 2,893, excluding those with primary CNS DLBCL). Two approaches were used to examine whether the long-term mortality of patients who responded to first-line therapy varied from that of the general population:
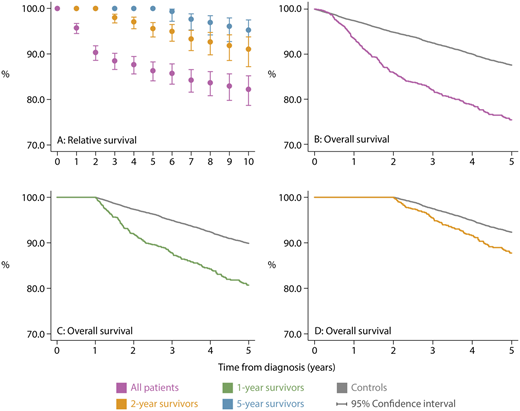
Relative Survival (RS, which adjusts for the age and sex specific mortality in the general population) was estimated using UK life tables to measure disease-specific survival.
For all patients diagnosed 2009-15 (cases, n=1,875), 10 people without DLBCL from the HMRN catchment population, matched on sex and year of birth, were selected (controls, n=18,750). Overall survival (OS) was estimated using standard statistical methods for both cases and controls. For controls the date of diagnosis of their matched case was used.
Mortality data (date and cause of death) for cases and controls were obtained from the Office for National Statistics - subjects were followed-up until June 2018 (median 6.8 years: range 2.8-13.7 years).
Results
Median age at diagnosis was 70.3 years, 68% of patients had an ECOG score of 0/1, 48% were diagnosed with stage IV disease and 28% had high risk disease as defined by the International Prognostic Index (IPI). The majority of patients were treated with intensive chemotherapy (n=2,355), predominantly R-CHOP (n=2,116); the remaining patients received non-intensive chemotherapy (2.2%), radiotherapy only (2%), or were managed with a supportive/palliative strategy (13.3%). As expected, those not treated curatively were, on average, older with a poorer performance status compared to those treated intensively (median age 80 years vs. 68 years, ECOG 0/1: 20% vs. 78% respectively).
For the 1,919/2,355 intensively treated patients who had either a complete or partial response their corresponding 1, 5, 10-year RS estimates from the time of diagnosis were 96%, 86% and 82% respectively (Figure A - purple marker). By contrast, the 1-year RS was 17% for those who did not achieve a response, either due to refractory disease or as a consequence of discontinuing first-line treatment (for any reason). The analyses were repeated to estimate RS for patients surviving 2-years (n=1,622) and 5-years (n=1,088) - 'conditional survival'. The corresponding 10-year RS estimates were 91% and 95% respectively.
Figures B-D show the Kaplan-Meier plots for cases diagnosed 2009-15 who achieved a response following intensive chemotherapy (n=1,254), as well as that of their corresponding age-sex matched controls (n= 12,540); 5-year OS was 75% and 88% respectively. The gap in 5-year OS between cases and controls narrowed when the analyses were repeated for cases and controls who survived 1 year after diagnosis: 79% (n=1,172) and 86% (n=12,218). The corresponding 2-year conditional survival estimates were closer still at 87% (n=1,006) and 89% (n=11,122) respectively.
Conclusion
In contrast to the small proportion of patients who did not respond to first-line therapy, the long term outlook for patients who responded to therapy were largely good, and any deaths that occurred were generally not attributable to lymphoma. Furthermore, encouragingly for patients who survived for at least 2 years after diagnosis, mortality almost returned to the background rate seen in the general population. These findings demonstrate that most patients diagnosed with DLBCL who are fit enough for treatment will be cured of their disease, regardless of their age at diagnosis.
Patmore:Gilead Sciences: Consultancy; Roche: Consultancy. Smith:Johnson & Johnson: Research Funding; Jazz Pharmaceuticals: Research Funding; Novartis: Research Funding; Gilead Sciences: Consultancy. Burton:NHS: Employment; Takeda: Honoraria; Roche: Honoraria; Takeda: Consultancy; Roche: Consultancy; Bristol-Myers Squibb: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.